Root Canal Treatment
Root Canal Treatment or Endodontics.
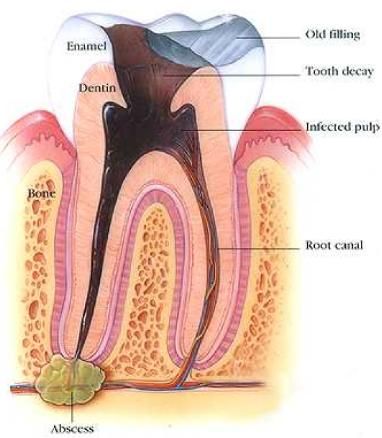
Your teeth are calcified objects with a hollow space within. The hollow space is known as the pulp chamber, which comprises of the nerves, arteries, veins, lymph vessels and connective tissue that nourish the tooth.
The nerve of each tooth enters at the tip of its root and runs through the centre of the root in small root canals that merge ultimately with the pulp chamber.
The number of canals varies according to the teeth. Generally, the front teeth have a single root canal while molars often have three or more canals.
A root canal treatment is performed when the pulp tissue of the tooth has become infected, this is done to prevent the formation of an abscess and the eventual spreading of the infection to the surrounding tissues.
If the tooth is left untreated it leads to the formation of an abscess, which is the collection of pus as a result of the multiplying bacteria, and it pushes beyond the root tips.
As the abscess expands within the bone, the tooth rises slightly out of its socket making it feel tender when you bite down. Without treatment, this infection can further spread to the surrounding tissues and nerves resulting in symptoms of: nausea, fever, and difficulty in swallowing.
Root canal treatment removes the infected pulp and disinfects the pulp chamber thereby stopping the spread and formation of further infection.
Root canal treatment can be required on a tooth for a variety of reasons, such as:
- Untreated tooth decay – causing bacteria to spread into your tooth and infect the pulp.
- Injury – a knock or blow to the tooth, which in turn affects and infects the pulp.
- Tooth breaks or fractures off at/near gum level. In order to build up with a retentive restoration (a post and crown), the tooth would first need to be root filled.
- Exposure of the nerve during routine dental treatment, if a cavity is quite deep, sometimes the nerve can become exposed when removing the decay.
What Are The Indications For A Root Canal Treatment?
By symptoms
- Persistent toothache.
- Presence of tenderness in your gums near a tooth.
- Presence of swelling in your gums near a tooth.
- A tooth that is partially or completely darkened following a trauma.
By dental examination
- X-rays – show a dark spot at the tip of the tooth’s root, indicating a reduction in the density of the bone surrounding the root’s tip as a result of the infection inside the tooth.
- Routine evaluation – a persistent or recurring pimple on your gums detected by the dentist.
- Due to exposure of a tooth’s nerve during dental work – may occur when the dentist is carrying out other dental work, in which case a root canal treatment may be necessary to prevent the degeneration of the tooth’s nerve tissue.
What are the Factors to Consider in a Root Canal Treatment?
Front teeth have fewer canals than the back teeth and hence the treatment for the former tends to be more successful.
Though re-treatment is possible for the same teeth, the margin of success reduces each time. We usually advise that this re-treatment be carried out by an endodontist which we can refer you to.
Complications although rare can occur in some cases.
Further dental work for restoring the functionality of the tooth
Usually the tooth that has undergone root canal treatment will require restorative dental work to make it sturdier. Also, restoration work helps to seal the teeth protecting its interior cavity from contamination by bacteria or other debris.
The common restoration recommended would be a post and crown. Some of the root filling material would need to be removed, this space created in the canal would allow a post to be placed. We use two systems for posts, one being placed at the chairside, the other requiring laboratory work. The overall restoration after post placement, would be a crown.